Important to safe guard
Diabetic Kidney Disease
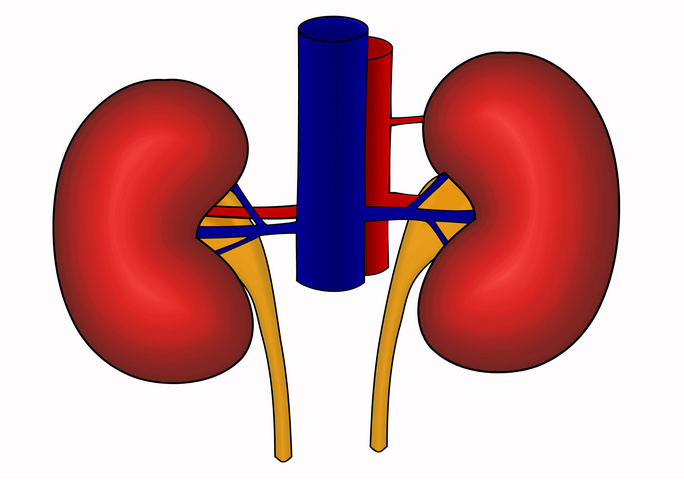
Your kidneys filter the blood and get rid of the waste products. Diabetics have a very high incidence of kidney disease. The earliest sign of diabetic kidney disease or nephropathy is microalbuminuria, which is the leakage of small amounts of protein in the urine. Your doctor would screen your urine yearly for microalbuminuria.
Gross protein loss (nephrotic syndrome) causes a decrease in albumin (protein) in the blood. This causes excessive fluid buildup or edema.
In more advanced kidney disease, the filters do not work properly, causing waste products in the blood. The build-up of waste products can cause nausea, vomiting, poor appetite, headaches, tiredness, easy bruising, and difficulty concentrating. Once the kidneys fail to filter, one may need hemodialysis or peritoneal dialysis, or a kidney transplant.
Prevention of diabetic kidney disease:
- Aim to keep your blood glucose levels as close to normal as possible. Based on several studies, good diabetic control certainly helps reduce or slow the progression of kidney disease.
- Blood pressure should be very well controlled, typically around 130/80 or less. Your doctor would very likely prescribe an Angiotensin-converting enzyme inhibitor (Example: Lisinopril, Enalapril, etc.), or he may prescribe an Angiotensin receptor blocker such as Irbesartan. Some people with diabetes may need more than one anti-hypertensive agent to lower blood pressure.
- Protein in the diet should be restricted. This is only recommended in severe kidney disease or eating a very high protein diet.
Be Informed. Get In Control. Prevent.
Better late than never
Need to Prevent
Kidney Disease In Diabetes
THE BURDEN OF KIDNEY FAILURE
Each year in the United States, more than 100,000 people are diagnosed with kidney failure, a serious condition in which the kidneys fail to rid the body of wastes.1 Kidney failure is the final stage of chronic kidney disease (CKD).
Diabetes is the most common cause of kidney failure, accounting for nearly 44 percent of new cases.1 Even when diabetes is controlled, the disease can lead to CKD and kidney failure. Most people with diabetes do not develop CKD that is severe enough to progress to kidney failure. Nearly 24 million people in the United States have diabetes, 2 and nearly 180,000 people live with kidney failure as a result of diabetes.1
People with kidney failure undergo either dialysis, an artificial blood-cleansing process, or transplantation to receive a healthy kidney from a donor. Most U.S. citizens who develop kidney failure are eligible for federally funded care. In 2005, care for patients with kidney failure cost the United States nearly $32 billion.1
Source: United States Renal Data System. USRDS 2007 Annual Data Report.
African Americans, American Indians, and Hispanics/Latinos develop diabetes, CKD, and kidney failure rates higher than Caucasians. Scientists have not been able to explain these higher rates. Nor can they explain fully the interplay of factors leading to kidney disease of diabetes—factors including heredity, diet, and other medical conditions, such as high blood pressure. They have found that high blood pressure and high blood glucose levels increase the risk that a person with diabetes will progress to kidney failure.
The United States Renal Data System. USRDS 2007 Annual Data Report. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, U.S. Department of Health and Human Services; 2007.
2National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics, 2007. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services, 2008.
The Course of Kidney Disease
Diabetic kidney disease takes many years to develop. In some people, the kidneys’ filtering function is actually higher than normal in the first few years of their diabetes.
Over several years, people developing kidney disease will have small amounts of the blood protein albumin begin to leak into their urine. This first stage of CKD is called microalbuminuria. The kidney’s filtration function usually remains normal during this period.
As the disease progresses, more albumin leaks into the urine. This stage may be called macroalbuminuria or proteinuria. As the amount of albumin in the urine increases, the kidneys’ filtering function usually begins to drop. The body retains various wastes as filtration falls. As kidney damage develops, blood pressure often rises as well.
Overall, kidney damage rarely occurs in the first 10 years of diabetes. Usually, 15 to 25 years will pass before kidney failure occurs for people who live with diabetes for more than 25 years without any signs of kidney failure—the risk of ever developing decreases.
DIAGNOSIS OF CKD
People with diabetes should be screened regularly for kidney disease. The two key markers for kidney disease are eGFR and urine albumin.
- eGFR. eGFR stands for estimated glomerular filtration rate. Each kidney contains about 1 million tiny filters made up of blood vessels. These filters are called glomeruli. Kidney function can be checked by estimating how much blood the glomeruli filter in a minute. The calculation of eGFR is based on creatinine, a waste product found in a blood sample. As the level of creatinine goes up, the eGFR goes down.
Kidney disease is present when eGFR is less than 60 milliliters per minute.
The American Diabetes Association (ADA) and the National Institutes of Health (NIH) recommend that eGFR be calculated from serum creatinine at least once a year in all people with diabetes.
- Urine albumin. Urine albumin is measured by comparing the amount of albumin to creatinine in a single urine sample. When the kidneys are healthy, the urine will contain large amounts of creatinine but almost no albumin. Even a small increase in the ratio of albumin to creatinine is a sign of kidney damage.
Kidney disease is present when urine contains more than 30 milligrams of albumin per gram of creatinine, with or without decreased eGFR.
The ADA and the NIH recommend annual urine albumin excretion assessment to assess kidney damage in all people with type 2 diabetes and people who have had type 1 diabetes for 5 years or more.
If kidney disease is detected, it should be addressed as part of a comprehensive approach to the treatment of diabetes.
EFFECTS OF HIGH BLOOD PRESSURE
High blood pressure, or hypertension, is a major factor in developing kidney problems in people with diabetes. Both a family history of hypertension and the presence of hypertension appear to increase the chances of developing kidney disease. Hypertension also accelerates the progress of kidney disease when it already exists.
Blood pressure is recorded using two numbers. The first number is called systolic pressure, and it represents the pressure in the arteries as the heartbeats. The second number is called the diastolic pressure, and it represents the pressure between heartbeats. In the past, hypertension was defined as blood pressure higher than 140/90, said “140 over 90.”
The ADA and the National Heart, Lung, and Blood Institute recommend that people with diabetes keep their blood pressure below 130/80.
Hypertension can be seen as a cause of kidney disease and as a result of damage created by the disease. As kidney disease progresses, physical changes in the kidneys lead to increased blood pressure. Therefore, a dangerous spiral involving rising blood pressure and factors that raise blood pressure occurs. Early detection and treatment of even mild hypertension are essential for people with diabetes.
PREVENTING AND SLOWING KIDNEY DISEASE
BLOOD PRESSURE MEDICINES
Scientists have made great progress in developing methods that slow the onset and progression of kidney disease in people with diabetes. Drugs used to lower blood pressure can slow the progression of kidney disease significantly. Two types of drugs, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), have proven effective in slowing kidney disease progression. Many people require two or more drugs to control their blood pressure. In addition to an ACE inhibitor or an ARB, a diuretic can also be useful. Beta-blockers, calcium channel blockers, and other blood pressure drugs may also be needed.
An example of an effective ACE inhibitor is lisinopril (Prinivil, Zestril), which doctors commonly prescribe for treating kidney disease of diabetes. The benefits of lisinopril extend beyond its ability to lower blood pressure: it may directly protect the kidneys’ glomeruli. ACE inhibitors have lowered proteinuria and slowed deterioration even in people with diabetes who did not have high blood pressure.
An example of an effective ARB is losartan (Cozaar), which has also been shown to protect kidney function and lower the risk of cardiovascular events.
Any medicine that helps patients achieve a blood pressure target of 130/80 or lower provides benefits. Patients with even mild hypertension or persistent microalbuminuria should consult a health care provider about the use of antihypertensive medicines.
MODERATE-PROTEIN DIETS
In people with diabetes, excessive consumption of protein may be harmful. Experts recommend that people with kidney disease of diabetes consume the recommended dietary allowance for protein but avoid high-protein diets. For people with greatly reduced kidney function, a diet containing reduced amounts of protein may help delay the onset of kidney failure. Anyone following a reduced-protein diet should work with a dietitian to ensure adequate nutrition.
INTENSIVE MANAGEMENT OF BLOOD GLUCOSE
Antihypertensive drugs and low-protein diets can slow CKD. A third treatment, known as intensive management of blood glucose or glycemic control, has shown great promise for people with diabetes, especially those in the early stages of CKD.
The human body normally converts food to glucose, the simple sugar that is the main energy source for the body’s cells. To enter cells, glucose needs the help of insulin, a hormone produced by the pancreas. When a person does not make enough insulin or does not respond to the insulin that is present, the body cannot process glucose, and it builds up in the bloodstream. High levels of glucose in the blood lead to a diagnosis of diabetes.
Intensive blood-glucose management is a treatment regimen that aims to keep blood glucose levels close to normal. The regimen includes testing blood glucose frequently, administering insulin throughout the day based on food intake and physical activity, following a diet and activity plan, and regularly consulting a healthcare team. Some people use an insulin pump to supply insulin throughout the day.
Several studies have pointed to the beneficial effects of intensive management of blood glucose. In the Diabetes Control and Complications Trial supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), researchers found a 50 percent decrease in early diabetic kidney disease development in participants who followed an intensive regimen for controlling blood glucose levels. The intensively managed patients had average blood glucose levels of 150 milligrams per deciliter-about 80 milligrams per deciliter lower than the conventionally managed patients’ levels. The United Kingdom Prospective Diabetes Study, conducted from 1976 to 1997, showed conclusively that, in people with improved blood glucose control, the risk of early kidney disease was reduced by a third. Additional studies conducted over the past decades have clearly established that any program resulting in sustained lowering of blood glucose levels will be beneficial to patients in the early stages of CKD.
Dialysis and Transplantation
When people with diabetes experience kidney failure, they must undergo either dialysis or a kidney transplant. As recently as the 1970s, medical experts commonly excluded people with diabetes from dialysis and transplantation because the experts felt damage caused by diabetes would offset the benefits of the treatments. Today, because of better control of diabetes and improved survival rates following treatment, doctors do not hesitate to offer dialysis and kidney transplantation to people with diabetes.
Currently, the survival of kidneys transplanted into people with diabetes is about the same as transplants’ survival in people without diabetes. Dialysis for people with diabetes also works well in the short run. Even so, people with diabetes who receive transplants or dialysis experience higher morbidity and mortality because of coexisting complications of diabetes, such as damage to the heart, eyes, and nerves.
GOOD CARE MAKES A DIFFERENCE
People with diabetes should
- have their health care provider measure their A1C level at least twice a year. The test provides a weighted average of their blood glucose level for the previous 3 months. They should aim to keep it at less than 7 percent.
- Work with their health care provider regarding insulin injections, medicines, meal planning, physical activity, and blood glucose monitoring.
- Has their blood pressure checked several times a year? If blood pressure is high, they should follow their health care provider’s plan for keeping it near normal levels. They should aim to keep it at less than 130/80.
- Ask their health care provider whether they might benefit from taking an ACE inhibitor or ARB.
- Ask their health care provider to measure their eGFR at least once a year to learn how well their kidneys are working.
- Ask their health care provider to measure the amount of protein in their urine at least once a year to check for kidney damage.
- Ask their health care provider whether they should reduce the amount of protein in their diet and ask for a referral to see a registered dietitian to help with meal planning.
POINTS TO REMEMBER
- Diabetes is the leading cause of chronic kidney disease (CKD) and kidney failure in the United States.
- People with diabetes should be screened regularly for kidney disease. The two key markers for kidney disease are estimated glomerular filtration rate (eGFR) and urine albumin.
- Drugs used to lower blood pressure can slow the progression of kidney disease significantly. Two types of drugs, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), have proven effective in slowing kidney disease progression.
- In people with diabetes, excessive consumption of protein may be harmful.
- Intensive blood-glucose management has shown great promise for people with diabetes, especially those in the early stages of CKD.
HOPE THROUGH RESEARCH
The number of people with diabetes is growing. As a result, the number of people with kidney failure caused by diabetes is also growing. Some experts predict that diabetes soon might account for half the cases of kidney failure. In light of the increasing illness and death related to diabetes and kidney failure, patients, researchers, and health care professionals will continue to benefit by addressing the relationship between the two diseases. The NIDDK is a leader in supporting research in this area.
Several areas of research supported by the NIDDK hold great potential. The Discovery of ways to predict who will develop kidney disease may lead to greater prevention, as people with diabetes who learn they are at risk institute strategies such as intensive management of blood glucose and blood pressure control.
Participants in clinical trials can play a more active role in their own health care, gain access to new research treatments before they are widely available, and help others by contributing to medical research. For information about current studies, visit www.ClinicalTrials.gov.
The U.S. Government does not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this document are used only because they are considered necessary in the context of the information provided. If a product is not mentioned, the omission does not mean that the product is unsatisfactory.
For More Information
National Diabetes Information Clearinghouse
1 Information Way
Bethesda, MD 20892-3560
Phone: 1-800-860-8747
TTY: 1-866-569-1162
Fax: 703-738-4929
Email: ndic@info.niddk.nih.gov
Internet: www.diabetes.niddk.nih.gov
National Diabetes Education Program
1 Diabetes Way
Bethesda, MD 20892-3560
Phone: 1-800-438-5383
TTY: 1-866-569-1162
Fax: 703-738-4929
Email: ndep@mail.nih.gov
Internet: www.ndep.nih.gov
National Kidney Disease Education Program
3 Kidney Information Way
Bethesda, MD 20892
Phone: 1-866-4-KIDNEY (454-3639)
Email: nkdep@info.niddk.nih.gov
Internet: www.nkdep.nih.gov
American Diabetes Association
1701 North Beauregard Street
Alexandria, VA 22311
Phone: 1-800-342-2383
Email: AskADA@diabetes.org
Internet: www.diabetes.org
National Kidney Foundation
30 East 33rd Street
New York, NY 10016
Phone: 1-800-622-9010 or 212-889-2210
Fax: 212-689-9261
Internet: www.kidney.org
You may also find additional information about this topic by visiting MedlinePlus at www.medlineplus.gov.
This publication may contain information about medications. When prepared, this publication included the most current information available. For updates or questions about any medications, contact the U.S. Food and Drug Administration toll-free at 1-888-INFO-FDA (1-888-463-6332) or visit www.fda.gov. Consult your doctor for more information.
National Kidney and Urologic Diseases Information Clearinghouse
3 Information Way
Bethesda, MD 20892–3580
Phone: 1–800–891–5390
TTY: 1–866–569–1162
Fax: 703–738–4929
Email: nkudic@info.niddk.nih.gov
Internet: www.kidney.niddk.nih.gov
The National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health of the U.S. Department of Health and Human Services. Established in 1987, the Clearinghouse provides information about the kidneys and urologic system diseases to people with kidney and urologic disorders and their families, health care professionals, and the public. The NKUDIC answers inquiries, develops and distributes publications, and works closely with professional and patient organizations and Government agencies to coordinate resources about kidney and urologic diseases.
Both NIDDK scientists and outside experts carefully review publications produced by the Clearinghouse.
This publication is not copyrighted. The Clearinghouse encourages users of this publication to duplicate and distribute as many copies as desired.
NIH Publication No. 08-3925
September 2008
Page last updated: September 2, 2010
Screening For Diabetes
Diabetes Screening and Diagnosis Who Should Be Screened? Everyone aged 45 and older should be screened for diabetes or glucose abnormalities every three years. However, individuals at higher risk should begin screening...
Disaster Planning
you never know When Disaster Occurs Emergency Preparedness for People with Diabetes When natural disasters or emergencies strike—such as hurricanes, floods, wildfires, or power outages—being prepared can protect your...
Neuropathy
Important to reduce all risk factors Diabetic neuropathy Diabetic neuropathy, a common complication of diabetes, encompasses various types of nerve damage resulting from prolonged high blood sugar levels. It can affect...
Contact Us
The newsletter is only sent if there are any new blogs or articles added.