Important Features
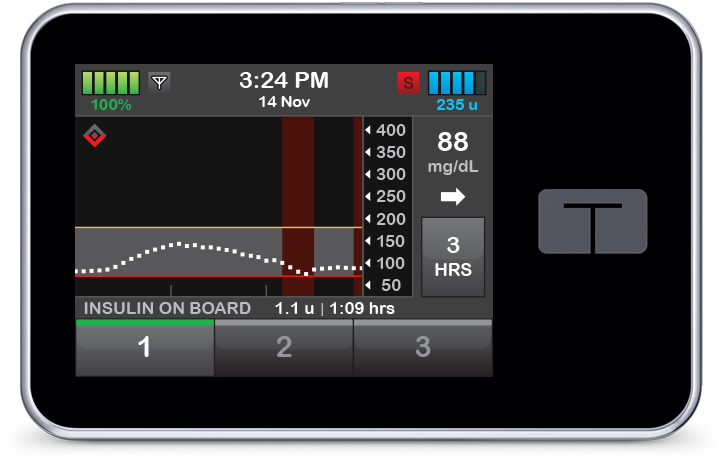
Insulin Pump
An insulin pump is a small, wearable device that helps people with diabetes manage their blood sugar levels by delivering insulin continuously throughout the day and night. This means you don’t have to give yourself multiple daily insulin injections.
How Does an Insulin Pump Work?
The pump delivers insulin in two main ways:
-
Basal Rate: A steady, low dose of insulin that’s delivered continuously to keep your blood sugar stable between meals and while you sleep.
-
Bolus Dose: Additional insulin you can program the pump to deliver at mealtimes or when your blood sugar is higher than your target range.
Insulin is delivered through a thin tube that connects the pump to a small needle or soft tube (called a cannula) inserted just under your skin, usually on your abdomen.
Types of Insulin Pumps
There are different types of insulin pumps available:
-
Tethered Pumps: These have a small tube connecting the pump to the cannula under your skin. The pump can be clipped to your belt or carried in a pocket. (Islet Bionic, T-slim, Medtronic pump).
-
Patch Pumps: These are tubeless and stick directly to your skin. They deliver insulin through a small cannula and are controlled wirelessly. (Omnipod).
Benefits of Using an Insulin Pump
-
Fewer Injections: With a pump, you avoid multiple daily injections.
-
Flexible Lifestyle: Pumps can make it easier to adjust insulin delivery for meals, exercise, and daily routines.
-
Better Blood Sugar Control: Pumps can help maintain more stable blood sugar levels, reducing the risk of highs and lows.
Considerations
Using an insulin pump requires commitment:
-
Regular Monitoring: You’ll need to check your blood sugar levels frequently to ensure the pump is delivering the right amount of insulin.
-
Site Changes: The infusion set (needle or cannula) needs to be changed every 2 to 3 days to prevent infections.
-
Technical Issues: Like any device, pumps can malfunction, so it’s important to have a backup plan, such as carrying insulin pens or syringes.
An insulin pump can be a valuable tool in managing diabetes, offering more flexibility and potentially better blood sugar control. However, it’s important to work closely with your healthcare team to determine if it’s the right choice for you and to learn how to use it effectively.
For a visual explanation, you might find this video helpful:
Be Informed. Get In Control. Prevent.
Better late than never
Our Blog
Follow Along
Disaster Planning
you never know When Disaster Occurs Emergency Preparedness for People with Diabetes When natural disasters or emergencies strike—such as hurricanes, floods, wildfires, or power outages—being prepared can protect your health and even save your life. Everyone with...
Neuropathy
Important to reduce all risk factors Diabetic neuropathy Diabetic neuropathy, a common complication of diabetes, encompasses various types of nerve damage resulting from prolonged high blood sugar levels. It can affect different parts of the nervous system, leading to...
Sick Day Management
What to do if you are under the weather Sick Day Management When you're sick with a cold, flu, or infection, your blood sugar levels can rise, potentially leading to serious health issues like diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS)....
Contact Us
The newsletter is only sent if there are any new blogs or articles added.