Another option
Surgery to Manage Diabetes
Bariatric Surgery |
|
|
Bariatric surgery may be the next step for people who remain severely obese after trying approaches other than surgery‚ especially if they have a disease linked to obesity. Severe obesity is a chronic condition that is hard to treat with diet and exercise alone. Bariatric surgery is an operation on the stomach and/or intestines that helps patients with extreme obesity to lose weight. This surgery is an option for people who cannot lose weight by other means or suffer from serious health problems related to obesity. The surgery restricts food intake, which promotes weight loss and reduces the risk of type 2 diabetes. Some surgeries also interrupt how food is digested, preventing some calories and nutrients, such as vitamins, from being absorbed. Recent studies suggest that bariatric surgery may even lower death rates for patients with severe obesity. The best results occur when patients follow surgery with healthy eating patterns and regular exercise. |
|
Bariatric Surgery for Adults |
Currently, bariatric surgery may be an option for adults with severe obesity. Body mass index (BMI), a measure of height about weight, is used to define levels of obesity. Clinically severe obesity is a BMI > 40 or a BMI > 35 with a serious health problem linked to obesity. Such health problems could be type 2 diabetes, heart disease, or severe sleep apnea (when breathing stops for short periods during sleep). RECENT DEVELOPMENTThe Food and Drug Administration (FDA) has approved the use of an adjustable gastric band (or AGB) for patients with BMI > 30 who also have at least one condition linked to obesity, such as heart disease or diabetes. Who is a good adult candidate for surgery?Having surgery to produce weight loss is a serious decision. Anyone thinking about having this surgery should know what it involves. Answers to the following questions may help patients decide whether weight-loss surgery is right for them. Is the patient:
There is no sure method, including surgery, to produce and maintain weight loss. Some patients who have bariatric surgery may have weight loss that does not meet their goals. Research also suggests that many patients regain some of the lost weight over time. The amount of weight regain may vary by extent of obesity and type of surgery. Habits such as snacking on foods high in calories or not exercising can affect weight loss and weight regain. Like a stretched pouch or separated stitches, problems that may occur with the surgery may also affect weight loss. Success is possible. Patients must commit to changing habits and having medical follow-up for the rest of their lives. |
Bariatric Surgery for Youth |
Rates of obesity among youth are high. Bariatric surgery is sometimes used to treat youth with extreme obesity. Although it is becoming clear that teens can lose weight after bariatric surgery, many questions still exist about the long-term effects on teens’ developing bodies and minds. Who is a good youth candidate for surgery?Experts in childhood obesity and bariatric surgery suggest that families consider surgery only after youth have tried for at least 6 months to lose weight and have not had success.1 Candidate should meet the following criteria:
Also, health care providers should assess potential patients and their parents to see how emotionally prepared they are for the surgery and the lifestyle changes they will need to make. Health care providers should also refer young patients to special youth bariatric surgery centers that focus on meeting youth’s unique needs. Mounting evidence suggests that bariatric surgery can favorably change both the weight and health of youth with extreme obesity. Over the years’ gastric bypass surgery has been the main operation used to treat extreme obesity in youth. An estimated 2,700 youth bariatric surgeries were performed between 1996 and 2003.2 A review of short-term data from the largest inpatient database in the United States suggests that these surgeries are safe for youth as adults. As yet, AGB has not been approved for use in the United States for people younger than 18. However, favorable weight-loss outcomes after AGB for youth have been reported abroad. |
The Normal Digestive Process |
Normally, as food moves along the digestive tract, digestive juices and enzymes digest and absorb calories and nutrients. After we chew and swallow our food, it moves down the esophagus to the stomach, where a strong acid continues the digestive process. The stomach can hold about 3 pints of food at one time when the stomach contents move to the duodenum (the first part of the small intestine), bile and pancreatic juice speed up digestion. Most of the iron and calcium in the food we eat is absorbed there. The other two parts of the small intestine’s nearly 20 feet absorb nearly all of the remaining calories and nutrients. The food particles that cannot be digested in the small intestine reside in the large intestine until eliminated. How does surgery promote weight loss?Bariatric surgery restricts food intake, which leads to weight loss. Patients who have bariatric surgery must commit to a lifetime of healthy eating and regular exercise. These healthy habits may help patients maintain weight loss after surgery. |
Types of Bariatric Surgery |
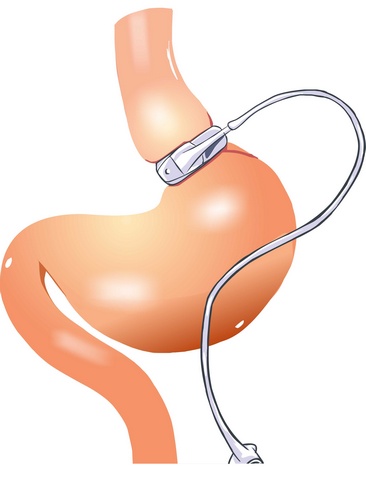
The type of surgery that may help an adult or youth depends on several factors. Patients should discuss with their health care providers what kind of surgery is suitable for them. What is the difference between open and laparoscopic surgery?Bariatric surgery may be performed through “open” approaches, which involve cutting the stomach in the standard manner, or by laparoscopy. With the latter approach, surgeons insert complex instruments through 1/2-inch cuts and guide a small camera that sends images to a monitor. Today, most bariatric surgery is laparoscopic because it requires a smaller cut, creates less tissue damage, leads to earlier hospital discharges, and has fewer problems, especially hernias occurring after surgery. However, not all patients are suitable for laparoscopy. Patients who are considered extremely obese, have had previous stomach surgery, or have complex medical problems may require the open approach. Complex medical problems may include having severe heart and lung disease or weighing more than 350 pounds. What are the surgical options?Four types of operations are commonly offered in the United States: AGB, Roux-en-Y gastric bypass (RYGB), biliopancreatic diversion with a duodenal switch (BPD-DS), and vertical sleeve gastrectomy (VSG). (See Figure 1.) Each surgery has its own benefits and risks. The patient and provider should work together to select the best option by considering each type of surgery’s benefits and risks. Other factors to consider include the patient’s BMI, eating habits, health conditions related to obesity, and previous stomach surgeries. FIGURE 1Diagram of Surgical Options. Image credit: Walter Pories, M.D. FACS. Adjustable Gastric BandAGB works mainly by decreasing food intake. Food intake is reduced by placing a small bracelet-like band around the stomach’s top to restrict the opening’s size from the throat to the stomach. The surgeon can then control the size of the opening with a circular balloon inside the band. This balloon can be inflated or deflated with a saline solution to meet the needs of the patient. |
Most weight loss
Gastric Bypass
Roux-en-Y Gastric BypassRYGB restricts food intake. RYGB also decreases how food is absorbed. Food intake is limited by a small pouch similar in size to the pouch created with AGB. Also, sending food directly from the pouch into the small intestine affects how the digestive tract absorbs food. The food is absorbed differently because the stomach, duodenum, and upper intestine no longer in contact with food. Biliopancreatic Diversion with a Duodenal SwitchBPD-DS, usually referred to as a “duodenal switch,” is a complex bariatric surgery that includes three features. One feature is to remove a large part of the stomach. This step makes patients feel full sooner when eating than they did before surgery. Feeling full sooner encourages patients to eat less. Another feature is re-routing food away from much of the small intestine to limit how the body absorbs food. The third feature changes how bile and other digestive juices affect the body’s ability to digest food and absorb calories. This step also helps lead to weight loss. In removing a large part of the stomach, the surgeon creates a more tubular “gastric sleeve” (also known as a VSG, discussed later). The smaller stomach sleeve remains linked to a concise part of the duodenum, directly linked to a lower part of the small intestine. This surgery leaves a small part of the duodenum available to absorb food and some vitamins and minerals. However, when the patient eats food, it bypasses most of the duodenum. The distance between the stomach and colon becomes much shorter after this operation, limiting how food is absorbed. BPD-DS produces significant weight loss. However, a decrease in the amount of food, vitamins, and minerals absorbed creates long-term problems. Some of these problems are anemia (lower than the normal count for red blood cells) or osteoporosis (loss of bone mass that can make bones brittle). Vertical Sleeve GastrectomyVSG surgery restricts food intake and decreases the amount of food used. Most of the stomach is removed during this surgery, which may decrease ghrelin, a hormone that prompts appetite. Lower amounts of ghrelin may reduce hunger more than other purely restrictive surgeries, such as AGB. VSG has been performed in the past mainly as the first stage of BPD-DS (discussed earlier) in patients who may be at high risk for problems from more extensive types of surgery. These patients’ high-risk levels are due to body weight or medical issues. However, more recent research indicates that some patients who have VSG can lose a lot of weight with VSG alone and avoid a second procedure. Researchers do not yet know how many patients who have VSG alone will need a second stage procedure. What are the side effects of these surgeries?Some side effects may include bleeding, infection, leaks from the site where the intestines are sewn together, diarrhea, and blood clots in the legs that can move to the lungs and heart. Examples of side effects that may occur later include poorly absorbed nutrients, especially in patients who do not take their prescribed vitamins and minerals. In some cases, if patients do not address this problem promptly, diseases may occur along with permanent damage to the nervous system. These diseases include pellagra (caused by lack of vitamin B3—niacin), beriberi (caused by lack of vitamin B1—thiamine), and kwashiorkor (caused by lack of protein). Other late problems include strictures (narrowing the sites where the intestine is joined) and hernias (part of an organ bulging through a weak muscle area). Two kinds of hernias may occur after a patient has bariatric surgery. An incisional hernia is a weakness that sticks out from the abdominal wall’s connective tissue and may cause a blockage in the bowel. An internal hernia occurs when the small bowel is displaced into pockets in the lining of the abdomen. These pockets occur when the intestines are sewn together. Internal hernias are thought to be more dangerous than incisional ones and need prompt attention to avoid serious problems. Some patients may also require emotional support to help them through body image changes and personal relationships that occur after the surgery. |
|
Medical Costs |
Bariatric procedures, on average, cost from $20,000 to $25,000. Medical insurance coverage varies by state and insurance provider. In 2004, the U.S. Department of Health and Human Services reduced barriers to obtaining Medicare coverage for obesity treatments. Bariatric surgery may be covered under these conditions:
Patients can contact staff at their regional Medicare, Medicaid, or health insurance office to determine if the procedure is covered and obtain facts about options. |
Research |
In 2003, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the NIH partnered with researchers to create the Longitudinal Assessment of Bariatric Surgery or LABS. LABS researchers are experts in bariatric surgery, obesity research, internal medicine, behavioral science, and related fields. Their mission is to plan and conduct studies that will lead to more knowledge about bariatric surgery and its impact on patients’ health and well-being with extreme obesity. More information about LABS is available at http://www.niddklabs.org. To help determine if bariatric surgery is appropriate for youth, NIH launched Teen-LABS in 2007. From 2007 to 2012, the multicenter study is collecting data from teens who plan to have surgery. The data will help to evaluate bariatric surgery’s benefits and risks. Researchers are collecting data about medical problems related to obesity, other health risk factors, and quality of life from these patients before surgery and 2 years after surgery. Researchers will then compare the teen outcomes to data from adults. These websites offer more information about Teen-LABS: http://www.nih.gov/news/pr/apr2007/niddk-16.htm and http://www.cincinnatichildrens.org/teen-LABS. |
Resources |
The following list of publications, websites, and organizations may be used for patients or health care providers discussing bariatric surgery. ADDITIONAL READING FROM THE WEIGHT-CONTROL INFORMATION NETWORKActive at Any Size. This fact sheet provides ideas and tips on how people considered to be overweight or obese can be physically active. It focuses on overcoming common barriers and setting goals. Available at http://www.win.niddk.nih.gov/publications/active.htm. Binge Eating Disorder. This fact sheet provides information and resources for patients who may have binge eating disorder. Available at http://www.win.niddk.nih.gov/publications/binge.htm. Dieting and Gallstones. This fact sheet explains what gallstones are, how they form, and the roles obesity and rapid weight loss play in developing gallstones. Available at http://www.win.niddk.nih.gov/publications/gallstones.htm. Weight Loss for Life. This booklet describes ways to lose weight and encourages healthy eating habits and regular physical activity. Available at http://www.win.niddk.nih.gov/publications/for_life.htm. ADDITIONAL READING FOR HEALTH CARE PROVIDERSPharmacological and Surgical Treatment of Obesity: Evidence Report/Technology Assessment: Number 103. Shekelle PG, Morton SC, Maglione M, et al. Agency for Healthcare Research and Quality (AHRQ). AHRQ Publication Number 04–E028–1; 2004. Rockville, MD. This report reviews the scientific evidence on weight-loss drugs and bariatric surgery among children, youth, and adults. Available at http://archive.ahrq.gov/clinic/epcsums/obesphsum.pdf [PDF – 441 Kb]. ADDITIONAL RESOURCEAmerican Society for Metabolic and Bariatric Surgery |
Weight-control Information Network1 WIN Way The Weight-control Information Network (WIN) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health, the Federal Government’s lead agency responsible for biomedical research on nutrition and obesity. Authorized by Congress (Public Law 103–43), WIN provides the general public, health professionals, the media, and Congress with up-to-date, science-based health information on weight control, obesity, physical activity, and related nutritional issues. Both NIDDK scientists and outside experts review publications produced by WIN. Walter Pories also reviewed this fact sheet, M.D.‚ FACS‚ Professor of Surgery and Biochemistry‚ Brody School of Medicine at East Carolina University; and Thomas Inge‚ M.D.‚ Ph.D.‚ FACS‚ FAAP‚ Assistant Professor of Surgery and Pediatrics and Surgical Director‚ Comprehensive Weight Management Center‚ Cincinnati Children’s Hospital Medical Center. This text is not copyrighted. WIN encourages unlimited duplication and distribution of this fact sheet. |
|
| U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 08–4006 March 2009 Updated June 2011 |
|
| References |
1. Inge TH‚ Krebs NF‚ Garcia VF‚ et al. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics. 2004 Jul;114(1):217–23. |
To contact WIN, call toll free 1–877–946–4627; fax: 202–828–1028; email: win@info.niddk.nih.gov;
or write Weight-control Information Network, 1 WIN Way, Bethesda, MD 20892–3665.
Be Informed. Get In Control. Prevent.
Better late than never
Coming Soon!
Available Aug 16, 2019
Diabetes Cure
Be Informed. Get In Control.

Our Blog
Follow Along
Screening For Diabetes
Diabetes Screening and Diagnosis Who Should Be Screened? Everyone aged 45 and older should be screened for diabetes or glucose abnormalities every three years. However, individuals at higher risk should begin screening earlier and more frequently—ideally once a year....
Disaster Planning
you never know When Disaster Occurs Emergency Preparedness for People with Diabetes When natural disasters or emergencies strike—such as hurricanes, floods, wildfires, or power outages—being prepared can protect your health and even save your life. Everyone with...
Neuropathy
Important to reduce all risk factors Diabetic neuropathy Diabetic neuropathy, a common complication of diabetes, encompasses various types of nerve damage resulting from prolonged high blood sugar levels. It can affect different parts of the nervous system, leading to...
Contact Us
The newsletter is only sent if there are any new blogs or articles added.